As told to Britt Julious
I think my story has a lot to do with learning about the medical industry and a lot about learning how to partner with your doctor. I learned a lot about cancer and the disease in regards to the origins of it. And so, that’s what that disease brought to me—figuring out how cancer came to my life and how it affected me. Straight from the beginning, I traced it back to almost 15 years ago, when this all started. I think my story has a lot to do with endurance, and has a lot to do with changing who I am.
It was really a process that unfolded really over six months. Initially, I felt cramps in my lower abdomen. I went to the urologist that was referred to me through my insurance. They performed a procedure, looked into my bladder and saw a dime-sized tumor. But at that point, they didn’t really suggest treatment. They just told me that I should take another look at it in three to six months.
But three months later, I started urinating blood. I met with a different urologist. She performed a cystoscopy. That’s where they take an exploratory view of your bladder. She immediately recommended we take it out and test it. So we got it tested and of course it came back positive for cancer. However, that doctor told me that they had it all and we kind of just moved on with life again.
Six months later, I was urinating blood again. The same urologist performed the test to see what was going on and still, no MRI and no CT scan was recommended. The doctor diagnosed me with a recurrence of the tumor, treated it, took it out and treated the surface of my bladder wall to see if there was any kind of cancer growth.
In the midst of that, I started developing a back pain essentially located in the spine. I met with an orthopedic doctor. He performed an MRI and noticed that the tumor wrapped around my spine and some [other] smaller tumors [were] near my ribs and liver. It was a bladder cancer that recurred and when we took it out, we didn’t realize it [had] invaded my muscle or my bladder wall. I had bladder cancer cells in my bone and in my liver. That’s when I received my full diagnosis of stage IV bladder cancer—transitional cell carcinoma.
We found every excuse in that process to not think that it was bladder cancer. I felt like the doctors were telling me what I wanted to hear, so I went along with it.
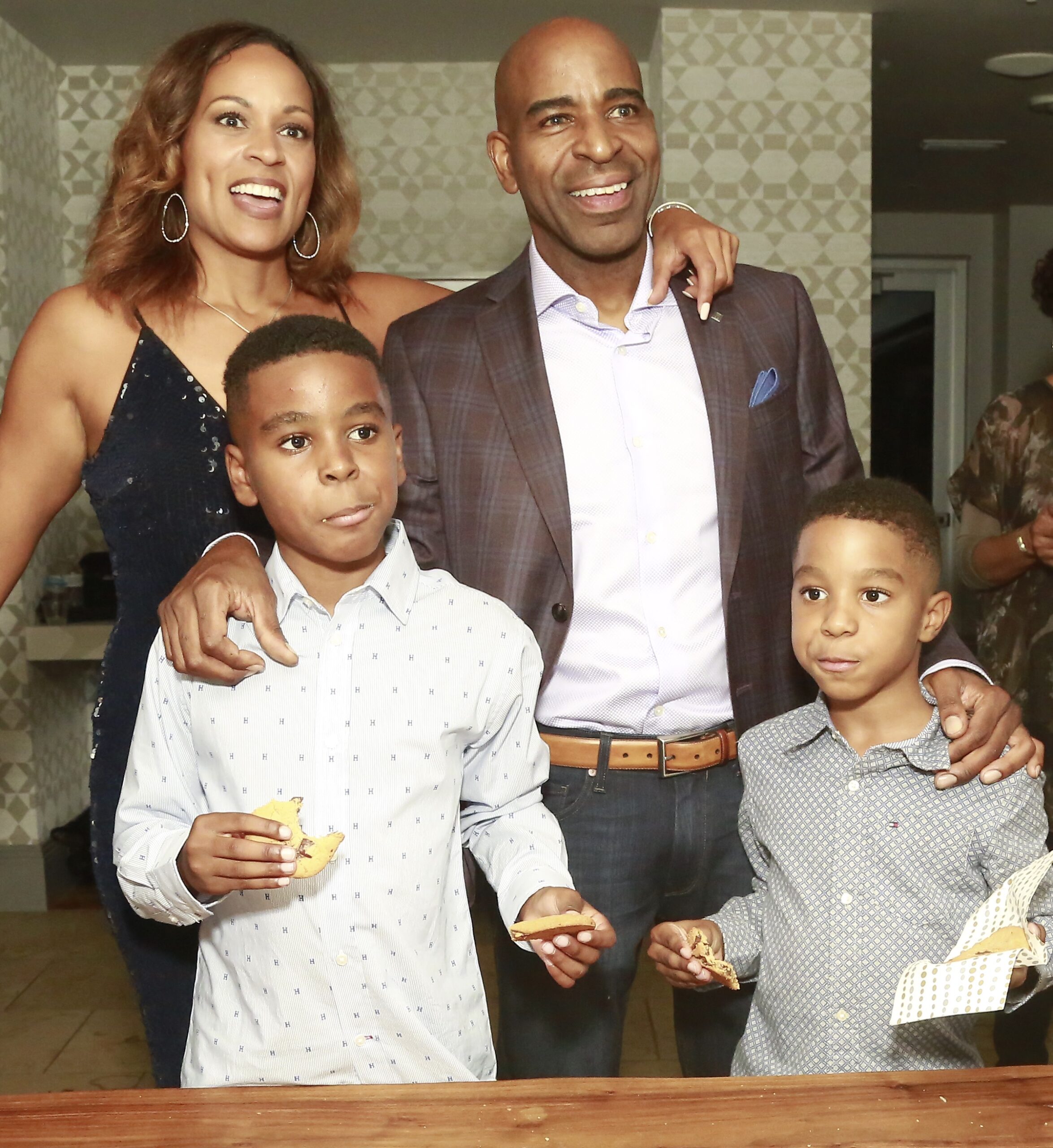
I didn’t want to accept that news. Before all of this, my significant other and I [were] fit folks. We have an exercise company. We eat well. Everything was perfect in our lives, so that was the last thing on our minds. When I originally urinated blood, I thought I burst a capillary. We went on a 15 mile hike and run that week in Austin and I thought maybe I just injured myself. We found every excuse in that process to not think that it was bladder cancer. I felt like the doctors were telling me what I wanted to hear, so I went along with it.
I was so afraid of what was going to happen to my family. I’m an introvert and my significant other is an extrovert. Socially, she has friends across the globe. She reached out to everyone against my will, quite honestly, to find out what are the options.
Our first [priority] was to find the less invasive process. We met with a radiation oncologist. Through that process, we thought maybe the radiation would slow the growth of the tumors. He talked about radiation and how diet, along with radiation, can accomplish some of the goals I wanted to accomplish. I [eventually] got 35 rounds of radiation, but during that time, the tumors increased in size and location. My health was deteriorating really fast. I was having extreme back pain. It got to the point where I couldn’t get out of bed to get to work. I had electrical shocks through my body.
My wife called EMS and they took me to the emergency room. They [finally] did a full body PET scan to see if I had any cancer cells in my brain. Luckily, no cancer cells were found in my brain. I found a statement that evening while I was in the emergency room that my life expectancy was six to nine months. And if the surgery was offered, [it was] to give me comfort through my final days. We felt like that was our option.
With my first surgical procedure, my doctor dug as much of the tumor out of my spine. Then, my spine [was reinforced] with metal rods to protect it from collapsing. After that surgery, I did six months in rehab followed by learning how to walk again. After the rehab, we had to decide on my actual cancer treatment. We were blessed with having a successful surgery. I was on a walker. At the time, I was 140 pounds. My body was extremely frail.
As a family, we didn’t feel my body was strong enough for platinum-based chemotherapy that was initially offered to me. Unfortunately, my platinum chemotherapy was the same platinum chemotherapy offered to my pops when he passed away from lung cancer. We felt like that was a sign. We came a long way in the last 30 years. We didn’t want to accept that. We didn’t think my body could withstand the treatment and thought quality would be better than quantity at the time.
My body was not acknowledging or recognizing the cancer cells in my body. It was having a party. It was calling friends and just growing and growing.
We pushed our doctor and we were on our second oncologist. We found an oncologist who was really a partner to us, who really listened to what our plan was going to be and was really open to treat our input with as much as we could. He did not scorn me for refusing the chemo. He didn’t aggressively say it was a bad idea. That was not his answer. He came back to us and said “You know what? Let’s give it a couple of more weeks and let’s keep looking.”
Later, he called us one day and said, “Hey, there’s a trial that’s been fast tracked through the FDA that might work. It’s specific for bladder cancer and its immunotherapy.”
It was right in line with everything I wanted to do, for the most part. We always viewed cancer for me as immune deficiency. I suffered before this cancer with arthritis and gout since I was 30 years old. I never took care of the root problem of the gout issue. I just masked it with other anti-inflammatory medicines that really [weren’t] helping my body at all. It was just masking the pain. So after years of that, my immune system was defeated. The cancer cell, as with any body, grows in the body and the duty of our immune system is to find it and defeat it. My body was not acknowledging or recognizing the cancer cells in my body. It was having a party. It was calling friends and just growing and growing. My body [wasn’t] acknowledging what was happening.
I thought it was a winner the second I saw it had immune in it. We feel like chemotherapy kind of napalms your body. We see immunotherapy more like an assistive therapy where the body can actually do for itself.
At first, I wasn’t sure if it had side effects or not because I wasn’t 100 percent at the time. But when I got strong enough and walked again, I was able to go to the gym after my treatment. I didn’t have the same side effects that other treatments may offer. I felt really fortunate about that.

I immediately showed progress and we started seeing tumors decrease until they disappeared. Now, I’m cancer free and it’s [been]at least two years now. We’re continuing with the therapy. I just completed my fourth year and I feel great.
I want people to first understand what cancer is for them. I think cancer is a real personal disease and it’s different for everyone. Although we go through a lot of the same things, it’s still different for everyone. I want them to know they are not helpless. They’re not at the mercy of one doctor. If you take an ownership role in this process, you can find a doctor that’s going to partner with you and understand what makes you tick and personalize the treatment for a disease that’s personal to you. I think there’s a lot of doctors out there that will do that. I’m lucky to have one that did that.
Be aware and in tune with your body. React quicker to the mild symptoms. Just don’t mask it. Figure out why it’s happening. You could be allergic to something. It could be the start of something small. But if you catch it early, that’s typically the best way to avoid cancer.
I hesitated to share because typically when you’re a cancer survivor, you tend to feel like that’s a lonely fight. And initially, that’s how I felt. Angry. Alone. However, when you dig and open up and share your story and allow people to understand what you’re going through, people are so willing to help and support. And that’s really what my story was about.







