With immunotherapy, healthy cells are trained to recognize and destroy cancer cells before they have a chance to spread.
Harnessing the body’s natural strength to fight disease is nothing new. Home remedies and holistic treatments have always been popular ways to jump-start the body’s ability to fight illness. Recently, immunotherapy—which bolsters the immune system to fine-tune an attack against illness rather than relying on external treatment methods—is gaining speed in cancer treatment. Cutting-edge developments are getting doctors closer than ever to a finalized treatment method, but the road to success has been a long one.
According to Dr. Leonard Lichtenfeld, Deputy Chief Medical Officer for the American Cancer Society, modern immunology began in the 1960s. “It’s not that we just discovered immunotherapy, it’s that it took us that long to develop our science to a point where we have treatments that are helpful to patients,” says Lichtenfeld. “Along the way, we had a lot of misfires.”
Immunotherapy treatments began as early as the late-19th century with the development of vaccines. Scientists Lewis Thomas and Frank Macfarlane Burnet turned the tides of cancer treatment research in 1957, when they suggested that white blood cells could identify and eliminate mutated cells. They dubbed this concept “cancer immunosurveillance,” and launched modern cancer immunotherapy efforts to fight cancer.
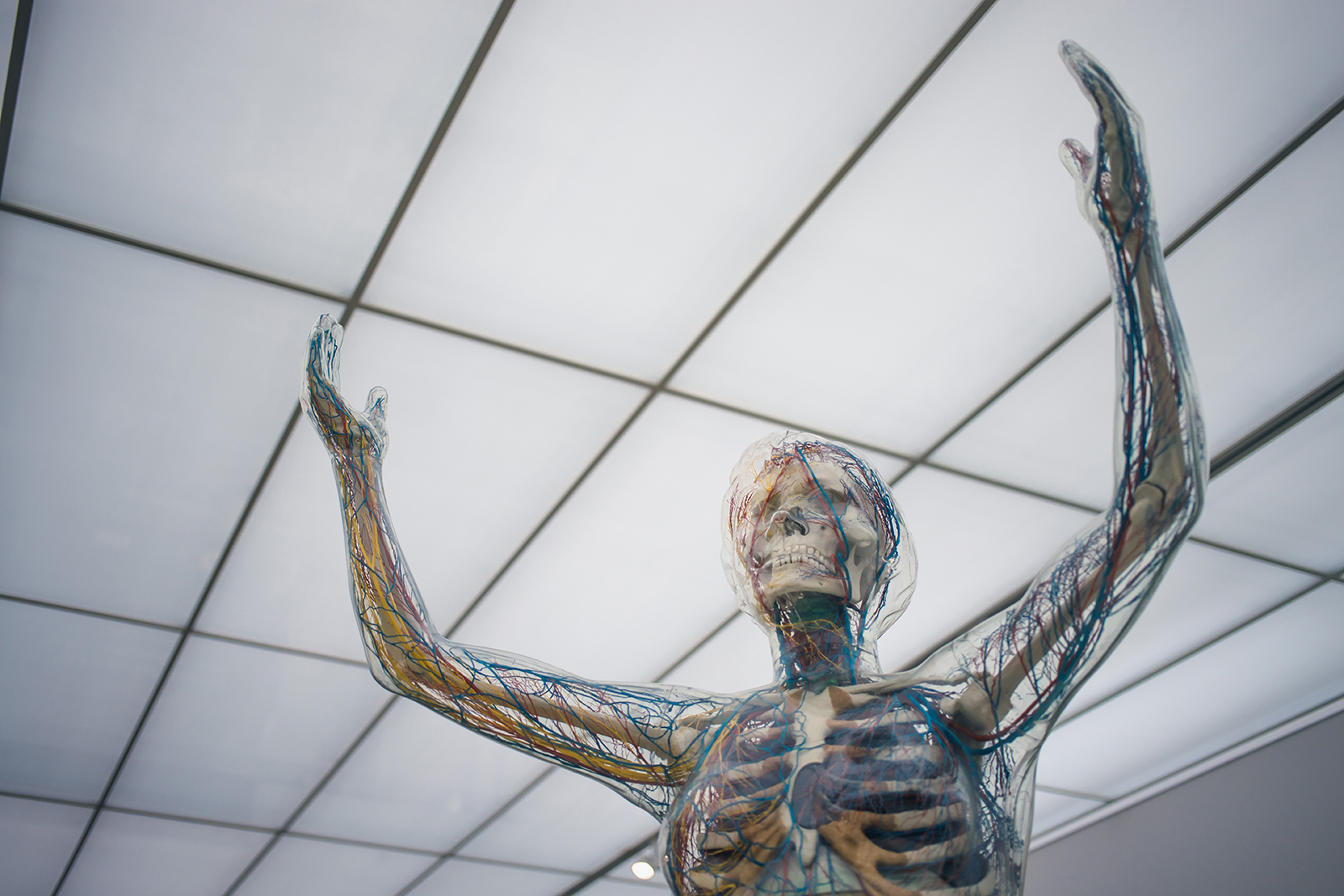
In aggressive cases, malignant cells evade the body’s defenses, allowing the cells to proliferate and develop into tumors. With immunotherapy, healthy cells are trained to recognize and destroy cancer cells before they have a chance to spread.
“We’re at a point now where immunotherapy is certainly a very exciting part of cancer treatment,” Lichtenfeld says. “Many of us suspect over time, it will have an even greater role as we learn more about how to use immunotherapy to reduce the burden of cancer.”
With immunotherapy, doctors hope to reduce the often intense side effects patients experience during chemotherapy and radiation. For most patients, nausea, vomiting, hair loss, and a lack of appetite can make the cancer treatment feel as debilitating to navigate as cancer itself. These side effects develop mainly due to the way chemotherapy works on a cellular level.
“Chemotherapy attacks cells in the body somewhat indiscriminately, [throwing] a monkey wrench into the cancer cells’ inner workings,” says Lichtenfeld. “[Chemotherapy] doesn’t do it very specifically. It doesn’t do it in a very targeted way, and in many situations, it hasn’t been very successful.”
Immunotherapy upends that system, creating highly specific and targeted immune system responses aimed at each patient’s particular cancer. Therapies such as CAR T-cell treatment deploy human-made antigen receptors explicitly designed to identify and latch onto flags in cancer cells. In one 2017 University of Chicago clinical trial, 70 to 90 percent of acute lymphoblastic lymphoma (ALL) patients went into remission following CAR T-cell therapy, and 40 to 50 percent of Non-Hodgkin lymphoma patients went into complete remission. A 2014 University of Chicago study treated relapsed and refractory, or chemo-resistant, ALL with CAR T-cell therapy and observed durable remissions up to 24 months. Such trials reflect recent efforts to use immunotherapy against chemo-refractory cancers, which do not respond to chemotherapy, or after chemotherapy attempts have failed in a patient.
However, researchers recommend caution. For some patients, the side effects can be severe or long-lasting. Because immunotherapy increases immune system activity, it holds the potential for overstimulation, which can lead to side effects like rheumatoid arthritis and inflammatory bowel disease or, in severe cases, death. Immunotherapy treatments are in constant development, and the long-term effects are mostly unknown. “It’s important to remember although immunotherapy has been beneficial for some patients, the majority of patients still do not benefit—in what I would call a meaningful way—from immunotherapy. There’s still a long way to go,” says Lichtenfeld.
Despite these complications, immunotherapy still holds great potential. In many patients, the immunotherpay-created cells survive and thrive long past the end of active treatment. In one clinical trial at Memorial Sloan Kettering, 50 percent of ALL patients in the low-disease category were in good health five years after CAR T-cell treatment. It appears immunotherapy may be able to rewire the body’s defenses and leave a patient stronger and more equipped to fight cancer cells in the future.
Some research suggests the most effective use of immunotherapy is in combination with traditional chemotherapy methods; the two treatments play on each other’s strengths and weaknesses to create a more effective treatment. In an ongoing Merck Sharp & Dohme Corp. study that began in 2016, advanced lung cancer patients who received a combination treatment had improved duration of tumor control and improved overall survival rates compared to patients who did not. According to Dr. Lichtenfeld, it is possible immunotherapy is more likely to work after chemotherapy weakens the cells.
“One theory is chemotherapy may not itself be very effective in killing as many cancer cells, but by disrupting the cell systems, it may make a cell more susceptible to immunotherapy,” says Lichtenfeld. “You have two drugs that are somewhat effective individually but are even more effective when used together.”
Lichtenfeld says theories like this pave the way for more innovative uses of immunotherapy in combination with other treatments. He is hopeful for a future of early-stage cancer detection in which immunotherapy becomes the first line of defense, with more invasive treatments used only if all else fails. Early studies at the American Society of Clinical Oncology suggest immunotherapy could function as the sole treatment of early-stage cancer. However, such developments remain primarily theoretical.
“We’re still very much in the learning phase, and we have to remember that it may not always be the answer for every patient,” Lichtenfeld says. “I am certainly hopeful, but we still have much more to learn.”